What is the HPO axis and how does it cause ovulatory dysfunction? And how does that relate to your missing or irregular period? These are all the questions we are going to answer in this article.
HPO axis is the complex communication that occurs between the hypothalamus, pituitary, and ovaries that ultimately is responsible for the hormones and neurotransmitters that control the menstrual cycle and ovulation.
When the communication breaks down between the members of the HPO axis, you end up with ovulatory dysfunction. As a result, women with ovulatory dysfunction ovulate irregularly or infrequently. There are several types of ovulatory dysfunction we’ll cover. But first, how do you know if you are even ovulating?
Do you have ovulatory dysfunction?
Before we get into the nitty gritty of HPO axis and ovulatory dysfunction. We first need to ask – are you ovulating?
Determining if you are ovulating regularly (or at all) is the central question of whether or not you have ovulatory dysfunction.
And note, just because you have a period does not mean that you are ovulating. Here are a few ways you can tell if you’re ovulating.
Use basal body temperatures (BBT) to track for a temperature shift post ovulation. Your body’s BBT will increase 0.5-1°F after ovulation and remain elevated until the start of your next bleed.
- Ask your doctor to do a progesterone lab test 5-7 days after you suspect you’ve ovulated or about 7 days before you expect your next period. Progesterone is only produced AFTER ovulation.
- You can also test for progesterone at home using an at home kit such as Proov.
- So, if you are ovulating – great! That means your HPO axis is up and running. Yay!
If you are not ovulating, that means it’s time to do some investigating about where the communication breakdown is happening within your HPO axis. Let’s dive into that next.
Types of Ovulatory Dysfunction
Ovulatory dysfunction is a fancy name for not ovulating and according to the WHO, there are three main categories of ovulatory dysfunction related to the HPO axis (1).
Here I am going to break down the 3 categories of dysfunction (plus a bonus 4th reason you might not be ovulating, be sure to read to the end of the article for that!). Then, I’ll cover what testing might help you get to the right diagnosis plus an overview of how each condition is treated.
Ok, so here are the 3 categories of ovulatory dysfunction according to the WHO:
- Hypothalamic Pituitary Failure
- Eugonadal Ovulatory Dysfunction
- Ovarian Failure
Let’s break them down.
Hypothalamic Pituitary Failure
First, hypothalamic pituitary failure (HPF). This accounts for about 10% of ovulatory dysfunction and is largely caused by genetics, congenital issues or from some kind of trauma (2).
With HPF, there is some kind of communication failure between the hypothalamus and pituitary gland. So the ovaries never get any kind of messaging that ovulation should happen.
Women with HPF likely had delayed puberty or currently have no cycle whatsoever. Investigating this type of ovulatory dysfunction usually includes checking labs such as FSH, LH, and estradiol. If HPF is suspected, it might also mean an MRI to take a look at the pituitary gland.
Unfortunately, there really aren’t any diet or lifestyle interventions to improve HPF and will require some kind of medical management.
Eugonadal Ovulatory Dysfunction
Next up, eugonadal ovulatory dysfunction. This is the most common type of ovulatory dysfunction, with about 85% of issues with ovulation coming from this category. This type of ovulatory dysfunction is caused by issues with endocrine messengers, which ultimately stop or delay ovulation (2).
Here are the most common conditions that fall within this category:
- Polycystic Ovarian Syndrome (PCOS) – for most women with this condition, blood sugar dysregulation and high insulin levels ultimately lead to irregular or skipped ovulation.
- Hypothyroidism – the thyroid hormone is crucial for a healthy cycle and a sluggish thyroid can slow or stop your cycle. Evaluation of the thyroid requires a FULL thyroid panel and working with a practitioner who can interpret labs in a way that relates to your menstrual cycle.
- Hypothalamic Amenorrhea (HA) – this is when a stress (either physical, emotional, or psychological) causes the hypothalamus to get off line and stop sending out signals that lead to ovulation. Undereating, low body fat, and over exercising are the most common stresses that lead to this condition. If undereating, low body fat, or over exercising are the cause for HA, increasing calorie intake, body fat, or reducing exercise will kickstart your cycle.
- Obesity – This one is tricky because excess weight can stop ovulation because of the hormonal activity of adipose (fat) cells. That being said, I think it is also important to point out that dieting is not the best approach to overcome this… because, see above (hypothalamic amenorrhea). A well-rounded and nourishing eating routine will help significantly more than any single “diet”.
- High prolactin levels – prolactin is high in breastfeeding women, but when it is high outside of breastfeeding, it can put the kibosh on ovulation (for the same reason women usually don’t ovulate when exclusively breastfeeding). When prolactin is high outside of breastfeeding, there are several causes that can be examined by your doctor with various treatment options including medication or potentially surgery.
Primary Ovarian Insufficiency or Failure
And the third and final category of ovulatory dysfunction is called primary ovarian insufficiency (POI) or failure (POF). And like the name implies, this is when the ovaries are offline and not properly functioning. About 5% of ovulatory dysfunction is caused by this category (2).
POI often has auto immunity at its root, though other conditions such as Turner syndrome/ other genetic conditions or toxic exposure can also be the cause.
Typically, your doctor will run certain tests to determine if POI/ POF is the reason you aren’t ovulating. This usually includes FSH, estradiol, AMH, and antral follicle count.
Because auto immunity is often at the root of POI, it’s important that I bring up gut health – which is often associated with autoimmunity (3).
There are lots of new research showing that improving gut health can help to reverse all kinds of autoimmune conditions, including POI! This is super exciting stuff and if POI ends up being the reason you aren’t ovulating, working with a skilled gut health practitioner might be just the ticket to help you conceive naturally.
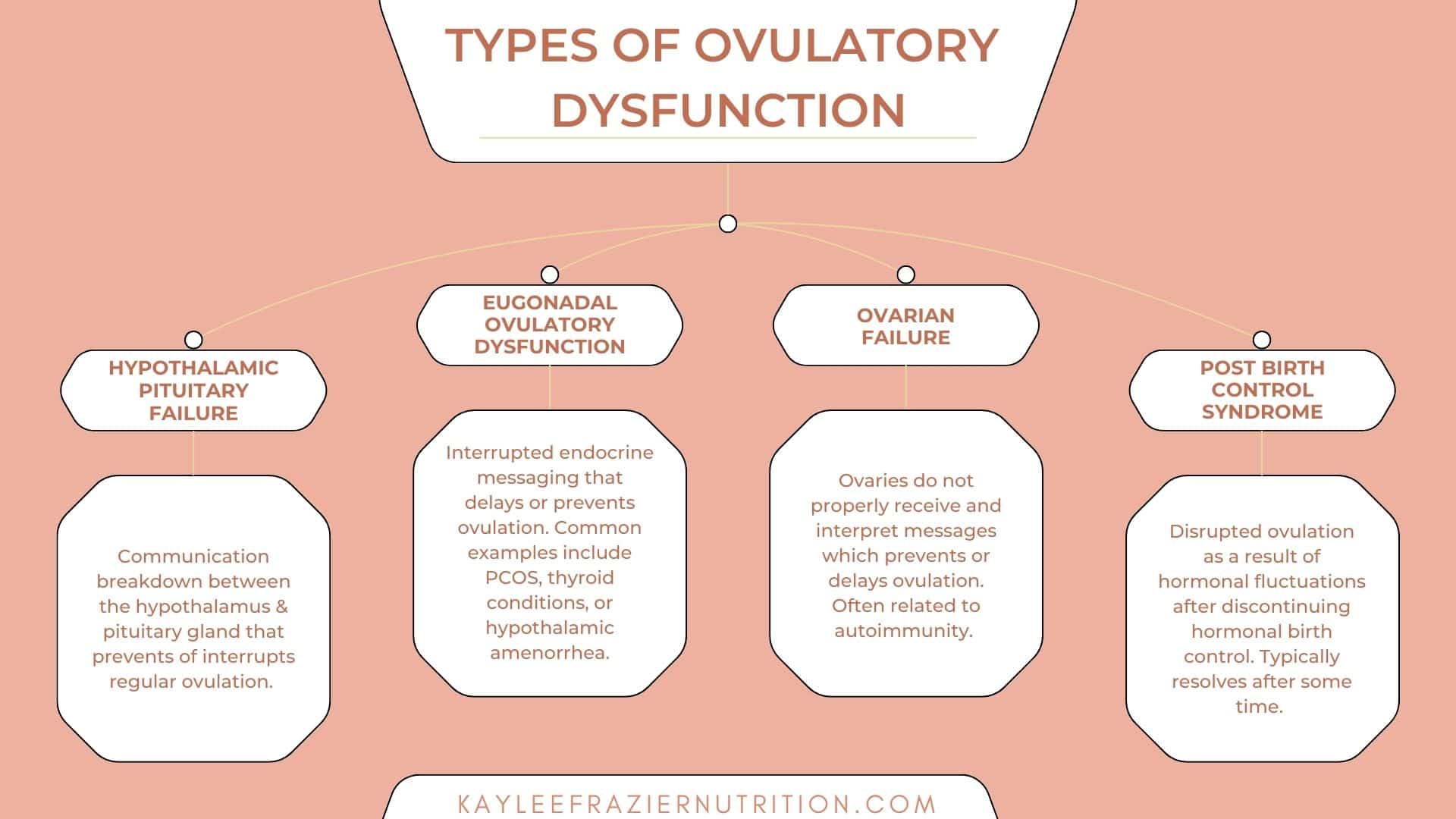
And one more possible reason you aren’t ovulating…
As promised – there is a 4th possible reason you aren’t ovulating regularly or at all. It is called Post Birth Control Syndrome (PBCS).
PBSC happens after you stop taking birth control. It includes a slew of symptoms such as missing/ irregular periods, heavy periods, crazy PMS, acne, headaches, hair loss, and more.
The good news, the cause of this hormonal imbalance is temporary and typically resolves after some time. Though, focusing on diet and lifestyle changes can help to speed the process and get you bad to a regular cycle (and optimal fertility!) as quickly as possible!
Final Thoughts
When you are trying to get to the bottom of an issue with your cycle, the first step is to determine whether or not you are ovulating. This will be a valuable piece of information to help your practitioner narrow in on the root cause for you cycle.
There are three main types of ovulatory dysfunction, and each has their own set of characteristics and treatment options. If you’ve determined that you are not ovulating, then it is time to dig in and figure out why.
Luckily there are many powerful diet and lifestyle interventions that can help with the most common causes of ovulatory dysfunction. Working with a skilled practitioner will allow you to learn the root cause for your ovulatory dysfunction and help you set up a diet and lifestyle plan targeted at the root cause of the dysfunction.
