If you’ve ever felt like your hormones are running the show—dictating your mood, energy, metabolism, and even your skin—you’re not alone. Hormonal imbalances can feel frustrating, unpredictable, and downright exhausting.
But here’s the good news: functional nutrition is a powerful tool to help you naturally get those hormones back into perfect harmony so you can go on living your best life.
Functional nutrition is a special type of nutrition approach that looks for root-causes of common ailments, including hormone dysfunction. With a functional nutrition approach, you learn how food, lifestyle, and targeted nutrients can optimize your hormone function.
Whether you’re dealing with estrogen dominance, adrenal fatigue, PCOS, or irregular cycles, functional nutrition helps you learn how to nourish your body. And this can make all the difference.
In this guide, we’ll break down how functional nutrition supports hormone health, the key foods and nutrients to focus on, and the lifestyle shifts that can help you feel your best. Plus, I’ll share how you can take your first steps towards a functional nutrition approach for hormone health.
What is Functional Nutrition?
Functional medicine takes a root-cause approach, looking beyond surface level symptoms to address the deeper imbalances driving them. As a whole, functional medicine focuses more broadly on several areas of health including genetics, lifestyle, and environment.
Functional nutrition is a very important sect of functional medicine that specifically focuses on understanding how food interacts with your body’s unique biochemistry to optimize hormone function, metabolism, and overall health.
Working within a functional nutrition model means going a lot deeper than a one-size-fits-all diet. So, rather than just prescribing a “healthy diet”, functional nutrition practitioners focus on:
- Supporting foundational systems such as gut health, blood sugar balance, stress response systems, and detox pathways.
- Addressing imbalances that are causing a symptom rather than just managing the symptom.
- Creating a personalized nutrition plan that targets your body’s individual needs.
In order to gain information to create individualized care plans, functional nutrition practitioners will often use functional lab testing. This may include special hormone testing, micronutrient panels, and other biomarkers that allow practitioners to make personalized recommendations. We’ll cover this in more detail later on.
While the idea of food as medicine is an ancient concept, the actual practice of functional medicine and functional nutrition is still considered a newly emerging field. And one that holds a lot of promise for helping women optimize their hormone health.
How Hormones Impact Your Health
Now that we understand functional nutrition, let’s talk more about hormones and your health.
Hormones are the body’s chemical messengers, influencing everything from metabolism and energy levels to mood, digestion, and reproductive health. When they’re balanced, you feel strong, energized, and in sync.
But when they’re out of balance, symptoms like fatigue, weight fluctuations, mood swings, and irregular cycles can start to appear. There are 4 key hormone systems that are impacted by nutrition that we will cover here.
Sex Hormones: Estrogen, Progesterone, & Testosterone
Your sex hormones do more than regulate reproductive health—they also impact mood, metabolism, and inflammation.
Estrogen plays a crucial role in bone health, brain function, and cardiovascular support, but too much can lead to estrogen dominance symptoms like PMS, bloating, and heavy periods.
Progesterone, often called the “calming hormone,” helps balance estrogen, supports pregnancy, and regulates cycles. When levels are low, anxiety, irregular periods, and sleep disturbances can become common.
Testosterone, though often overlooked in women, is essential for muscle strength, libido, and energy. A deficiency can lead to fatigue and decreased motivation.
Adrenal Hormones: Cortisol & DHEA
Your adrenal glands produce hormones that help you respond to stress and regulate energy levels.
Cortisol, the body’s primary stress hormone, helps you wake up in the morning and adapt to daily challenges. However, chronic stress can lead to cortisol dysregulation, causing fatigue, weight gain, and blood sugar imbalances. Chronically elevated cortisol can also impact the levels of stress hormones leading to cycle irregularities.
DHEA another hormone that is largely made in the adrenal gland. It is the precursor to most of the sex hormones. It also plays a key role in resilience and vitality which is why low levels are linked with burnout and poor recovery from stress. DHEA is also crucial for healthy egg development and low levels are linked with poor egg quality.
Thyroid Hormones
The thyroid is the master regulator of metabolism, influencing body temperature, digestion, and mood.
There are two main forms of thyroid hormone. T3 is considered the active form of the hormone and T4 is a precursor hormone. Thyroid hormones control metabolic rate, energy production, and brain function. A poorly functioning thyroid leads to symptoms such as fatigue, weight gain, and sluggish digestion.
Insulin & Blood Sugar: Glucose Control & Metabolic Health
Insulin is essential for blood sugar regulation. It helps to shuttle glucose into the cells so the glucose can be burned for energy. But, imbalances in insulin levels lead to weight gain, cravings, and hormonal disruptions.
Insulin resistance is one of the most common hormone imbalances. It occurs when the body becomes less responsive to insulin. Because cells are not responding to normal levels of insulin, the body produces more and more in an effort to keep blood sugar stable. This is often seen in PCOS and causes erratic blood sugar levels, weight gain, and increased inflammation.
Poorly regulated blood sugar and insulin resistance can affect egg quality, ovulation, implantation, and even the health of a developing embryo.
Signs of Hormonal Imbalances
If you’ve struggled with hormonal imbalances, you know how frustrating they can be. These imbalances often show up as persistent symptoms—fatigue, mood swings, irregular cycles, or stubborn weight changes—without an obvious cause.
Many women experience the symptoms of estrogen dominance, adrenal fatigue, or blood sugar instability without realizing that their diet and lifestyle play a significant role in these imbalances.
And unfortunately, given the vagueness of the symptoms, many women struggle to get the help they need to heal from conventional medical providers. This is where a functional nutrition approach for hormone balance can really be life changing.
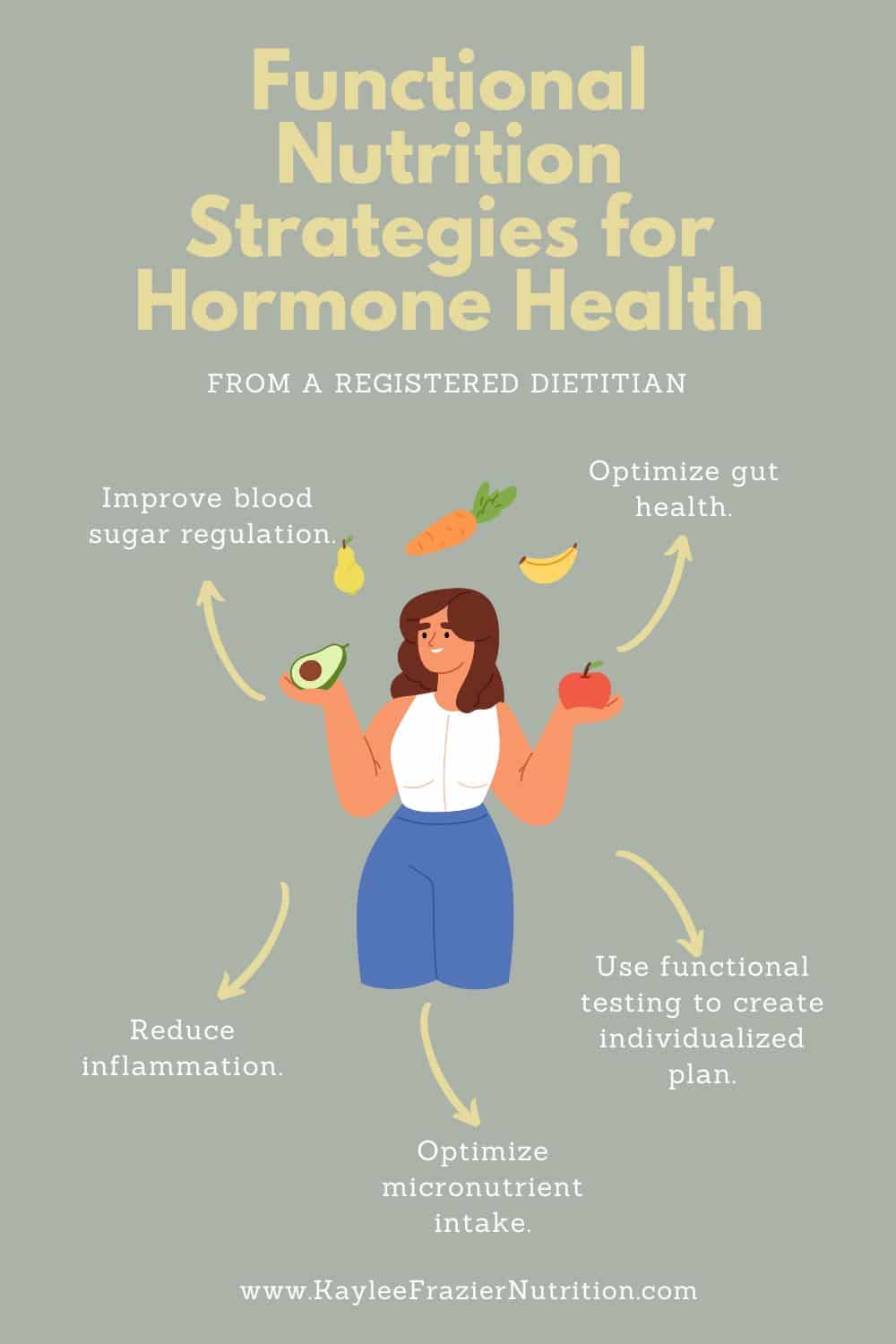
Functional Nutrition Strategies for Hormone Balance
Hormones don’t operate in isolation—they constantly respond to signals from food, stress, sleep, and environmental factors. That’s why a functional nutrition approach to hormone health focuses on the whole person, rather than just isolated symptoms.
Interventions may target systems that don’t seem directly related to fertility or reproductive health, but that’s because everything in the body is interconnected. Blood sugar regulation, gut health, detoxification, inflammation, and micronutrient status all send signals that influence hormone balance.
By addressing these foundational systems, functional nutrition helps restore equilibrium, supporting fertility, energy, and overall well-being. Below, we will cover some of the common functional nutrition strategies that are used to help with healthy hormone balance.
Blood Sugar Regulation
Balanced blood sugar is essential for hormone health. When glucose levels fluctuate wildly—spiking after meals and crashing soon after—it puts stress on the body, leading to insulin resistance, cortisol dysregulation, and estrogen imbalances.
Chronically high insulin levels can drive excess androgen production, which is often seen in PCOS, while blood sugar crashes can trigger adrenal stress and fatigue.
Functional nutrition focuses on stabilizing blood sugar through nutrient-dense meals that include protein, fiber, and healthy fats.
Gut Health
Your gut health plays a huge role in hormone balance, influencing everything from estrogen metabolism to cortisol regulation.
For example, a healthy microbiome helps process and eliminate excess hormones, particularly estrogen, through the estrobolome. The estrobolome is a collection of gut bacteria responsible for estrogen detoxification.
When gut health is compromised—due to dysbiosis, poor digestion, or inflammation—it can lead to hormonal imbalances and irregular cycles. There are many ways that functional nutrition supports gut health including an emphasis on fiber-rich foods, fermented foods, and prebiotics all of which nourish beneficial bacteria and improve digestion
Inflammation
Chronic inflammation disrupts hormone signaling, contributing to insulin resistance, thyroid dysfunction, and reproductive hormone imbalances.
Functional nutrition prioritizes anti-inflammatory foods, such as omega-3-rich fish, colorful vegetables, and polyphenol-packed berries. Avoiding inflammatory triggers—like excessive sugar, processed foods, and industrial seed oils—can help reduce inflammation and stabilize hormones.
Micronutrient Optimization
Hormones rely on specific vitamins and minerals to function properly. For example, magnesium supports progesterone production, zinc plays a role in testosterone balance, and vitamin D is essential for immune and reproductive health.
Functional nutrition ensures optimal micronutrient intake by focusing on nutrient-dense whole foods and, when necessary, targeted supplementation. Addressing deficiencies can improve cycle regularity, energy levels, and metabolic function, thereby creating a strong foundation for hormone balance.
Macronutrient Distribution & Meal Patterns
The way you structure meals and the breakdown of macronutrients in your overall diet play a crucial role in hormone health.
It is especially important to include enough protein and healthy fats in a hormone health diet. That is because these macronutrients stabilize blood sugar, support hormone production, and reduce inflammation.
Prioritizing adequate protein intake—from sources like grass-fed meats, eggs, fish, and legumes—ensures your body has the building blocks for hormone synthesis. Healthy fats, such as avocados, olive oil, nuts, and omega-3-rich fish, provide essential nutrients for hormone regulation.
Different eating patterns can serve as helpful frameworks for hormone balance. However, there is no single diet that fits everyone. Functional nutrition personalizes meal patterns based on individual needs, ensuring food choices work with hormone balance rather than against it.
Key Foods that Support Hormone Health
The food you eat sends powerful signals to your hormones, influencing metabolism and reproductive health. Certain foods contain unique compounds that help regulate hormone production and assist with detoxification.
By incorporating these nutrient-dense options into your diet, you can support your body’s natural ability to maintain hormonal equilibrium. Below are some foods that have unique and powerful impacts on your hormone health that should be considered as part of most hormone healing diets.
Cruciferous Vegetables: Supporting Estrogen Metabolism
Cruciferous vegetables—like broccoli, cauliflower, kale, and Brussels sprouts—contain indole-3-carbinol and sulforaphane. These compounds help the body process and eliminate excess estrogen by promoting healthy liver detoxification.
If estrogen dominance is contributing to symptoms like bloating, PMS, or irregular cycles, adding more cruciferous vegetables to your meals can be a simple yet effective way to support balance.
Healthy Fats: Omega-3s and Their Role in Hormone Production
Hormones are built from fats, making healthy fat intake essential for hormone production and function. However, many women underconsume fats, specifically omega-3 fatty acids.
Omega-3 fatty acids, found largely in wild-caught fish, help reduce inflammation and support hormone signaling. These fats also play a role in balancing cortisol levels, which can be especially helpful for managing stress-related hormone imbalances.
Other important fats include olive oil, avocado, nuts/ seeds, and animal fats from high quality animal sources. Eating plenty of fat ensures your body has the raw materials it needs for optimal hormone health.
Protein & Amino Acids: Stabilizing Blood Sugar and Providing Raw Building Material
Protein is a key player in hormone regulation because it helps to stabilize blood sugar and provides building blocks for key body compounds.
Blood sugar fluctuations can disrupt insulin levels, leading to hormonal imbalances that affect metabolism and reproductive health. Prioritizing high-quality protein sources—such as grass-fed meats, eggs, lentils, and bone broth—helps maintain steady energy levels and supports the production of important compounds such as glutathione.
Fermented Foods: Feeding the Microbiome
Your gut plays a huge role in hormone health, particularly in estrogen detoxification and absorption of key nutrients.
Fermented foods like sauerkraut, kimchi, yogurt, and kefir contain beneficial probiotics that support a healthy microbiome. A balanced gut microbiome helps regulate estrogen levels, which will reduce symptoms of estrogen dominance and supports overall hormone balance.

Functional Testing: Use Labs to Personalize Nutrition
When it comes to hormone health, using functional testing can be a game-changer. Instead of guessing what’s going on, functional testing provides real data that helps uncover imbalances and guides personalized nutrition strategies.
DUTCH Test
One of the most valuable tools for hormone testing is the DUTCH test, which offers a comprehensive look at sex hormones, adrenal function, and hormone metabolism.
The DUTCH test uses several urine samples collected throughout the day to assess hormone levels. Unlike standard blood tests that provide a snapshot of hormone levels at a single moment, the DUTCH test measures hormone fluctuations over a full day.
Another benefit of the DUTCH test is that it measures hormones and hormonal metabolites. This shows a larger picture of how hormones are flowing through metabolic pathways which can help to pinpoint where things may be going awry.
The DUTCH test can be especially helpful for identifying estrogen dominance, adrenal fatigue, and cortisol dysregulation, making it a powerful tool for tailoring nutrition and lifestyle interventions.
Micronutrient Testing
Micronutrient testing is another helpful testing option. Many hormonal imbalances stem from nutrient deficiencies, such as low magnesium, zinc, or vitamin D, which play critical roles in hormone production and metabolism.
Functional nutrition uses micronutrient testing to pinpoint gaps in a person’s diet and create targeted strategies to replenish essential nutrients.
Practitioners may use conventional blood panels to assess some micronutrients such as iron, vitamin D, or vitamin B12. But other micronutrients cannot be accurately assessed from conventional lab testing.
Therefore, functional practitioners may use organic acid tests (OATs), hair mineral analysis, or other specialized micronutrient testing to get a closer look at nutrient status. These tests typically need to be ordered outside of a conventional healthcare setting and are usually not covered by insurance.
Conventional Lab Testing
While conventional testing may not be the best option for assessing micronutrient status, there are still some powerful conventional lab tests that functional nutrition providers use. Tests such as thyroid panels and blood sugar markers can provide deep insights, especially when viewed through a functional nutrition lens.
For example, while standard thyroid testing often focuses on TSH alone, a functional approach looks at free T3, free T4, reverse T3, and thyroid antibodies to get a more complete understanding of thyroid function.
Similarly, fasting glucose, fasting insulin, and A1C levels can reveal early signs of insulin resistance, even before blood sugar issues become clinically significant.
When you work with a functional nutrition practitioner, they will be able to help you decide what additional testing will be helpful for you. Using the correct tests can be key to identify root causes and develop personalized interventions to heal.
Lifestyle and Environmental Factors
While nutrition is a powerful tool for hormone balance, it’s only one piece of the puzzle. We can’t forget about the importance of looking at our stress, sleep, environmental exposures, and movement when working on our hormone health.
Stress & Hormones
Chronic stress can seriously disrupt hormone balance. When stress levels remain high, the body produces excess cortisol, which can interfere with progesterone production, thyroid function, and blood sugar regulation.
Over time, this can lead to symptoms like fatigue, irregular cycles, and difficulty losing weight.
As part of a functional approach to hormone health, you may find it helpful to manage stress through mindful practices, nervous system regulation, and gratitude practice.
Sleep & Hormone Regulation
Sleep is non-negotiable when it comes to hormone health. Poor sleep quality or inconsistent sleep patterns can disrupt melatonin, cortisol, and reproductive hormone cycles, making it harder for the body to regulate metabolism and repair tissues.
Prioritizing consistent sleep schedules, reducing blue light exposure, and supporting circadian rhythms can improve hormone function and overall well-being.
Endocrine Disruptors & Toxic Exposures
Environmental toxins can interfere with hormone signaling. Endocrine disruptors—found in plastics, pesticides, and conventional beauty products—mimic hormones in the body and disrupt the normal hormone balance, hence the name endocrine disruptors.
Some of the best ways to reduce your exposure to endocrine disruptors and other toxic exposures include: choosing organic produce when possible, switching to non-toxic personal, and limiting the use of cleaning chemicals. You can search for cleaner personal care products and household cleaners on the Environmental Working Group’s website.
Exercise & Movement
The right type of movement can support hormone balance, while excessive or poorly timed exercise can increase stress hormones and disrupt overall hormone balance. Knowing what type of exercise routine is best for you ensures that your movement routine is helping to heal your hormones rather than hinder them.
For example, in women with PCOS strength training helps boost insulin sensitivity and supports metabolic health. And for women recovering from hypothalamic amenorrhea, gentle movement like walking or yoga will be the best option.
A functional approach to exercise focuses on individual needs, ensuring movement enhances hormone balance rather than working against it.
Conclusion & Next Steps
Functional nutrition offers a unique and powerful approach to hormone health. The main goal of a functional nutrition approach to hormone health includes identifying the root causes and creating an individualized care plan to target and resolve these issues.
Functional nutrition providers focus on rebalancing various systems in the body to naturally return hormones to their ideal balance. This may include reducing inflammation, supporting gut health, emphasizing detox pathways, or identifying nutrient gaps.
Oftentimes, functional nutrition providers will use functional tests to identify the root causes of hormone imbalances. The DUTCH test, micronutrient panels, and other conventional blood tests are all very useful.
The ultimate goal of a functional nutrition approach to hormone health is an individualized plan that will uniquely support each individual back to their ideal state of hormone balance.
Does a functional nutrition approach to hormone health sound like it might be right for you?
You can find a functional nutrition provider in the Integrative and Functional Nutrition directory and get started in your hormone healing journey today!
